Roger Davis Deutsch
CEO, Cell Sciences Systems (US) & ALCAT Europe
Abstract
The aging processes, described by Denham Harmon in the 1950s, are manifesting at earlier ages. Metabolic syndrome, characterized by obesity, diabetes, and cardiovascular disease, has sharply increased in recent years. Many observational studies support the thesis that the deleterious effects exerted by free radicals, upon lipid membranes, DNA, and protein structures, forms the common underlying basis of the many diverse degenerative aging disorders. The inability to tolerate foods and environmental factors induces chronic activation of the innate immune system and gives rise to inflammatory processes, which includes excess production of reactive oxygen species and the release of preformed and newly synthesized mediators of inflammation. A simple blood test (the Alcat Test) can be used to identify food and other factors that induce innate immune system activation. This review article describes the relationships between inflammatory processes, degenerative disorders, and dietary factors.
Keywords: nutrigenomics, metabolic syndrome, innate immunity, specific immunity, allergy, food Intolerance, food sensitivity
Introduction
Since the introduction of the free radical theory of aging by Denham Harmon in 1956(1) numerous findings have supported the notion that random damage induced by reactive oxygen species (ROS) exerts deleterious effects on a wide range of cellular and tissue structures resulting in degeneration and aging. On the other hand, it has also been demonstrated that certain foods containing sirtuins, such as resveratrol (found in red wine) can switch on the same genes that are activated during times of calorie restriction thereby exerting a regenerating effect, or down regulation of the P53 gene.(2)
Whilst other foods induce hormonal secretions associated with the activation of proinflammatory genes, such as foods having a high glycemic index that induce insulin secretion. It is quite possible that food induced inflammatory bowel promotes sugar cravings as activated immune cells in the gut consume serotonin, thus possibly creating a deficit of this key neurotransmitter in the brain.(3) Yet, other foods exert anti-inflammatory effects, such as foods high in n-3 fatty acids (EPA, DHA), e.g. oily fish, which induce a decrease in inflammatory cytokine production from monocytes, notably, IL-1, IL-6, and TNF-alpha.(4)
Chronic inflammation is the primary cause of free radical generation and the common soil of most, if not all, of the diseases of aging. The most significant source of free radicals, as well as preformed and newly synthesized inflammatory mediators, is the activated innate immune system. Further, clinical observations suggest a link between genetic differences and how each individual reacts to food and other environmental exposures as a function of biochemical individuality. Adverse reactivity to foods and other environmental substances activates the innate branch of the immune system, generating release of toxic inflammatory mediators and reactive oxygen and nitrogen species.
Chronic activation of innate immunity appears to underlie and form a common basis for a wide range of generative diseases associated with the aging; including, diabetes, obesity, cardiovascular disease, arthritis, dementia, auto-immunity, and others.
In some instances an infectious agent is demonstrable. However, in many cases no specific antibody is demonstrable and the inciting environmental factor is presumed to be other than microbial.
Commonly eaten, but constitutionally incompatible foods and additives, as well as other environmental exposures, seem to be associated with chronic activation of innate immunity and therefore a major contributor to degenerative processes.
Immunity
A basic review of salient features of the immune system, for the non-immunologist, is in order. Many authors have drawn military parallels describing the human immune system as being similar to a country’s defenses. Like a military organization, the immune system must function under tight regulation. If it breaks down, the effects may be devastating. An enemy might attack without resistance; or, the army might grossly overreact to a harmless situation, dropping bombs or launching missiles on a pack of boy scouts or a Salvation Army parade. Simple as it sounds, the military needs to react when it should, and not react when it shouldn’t. So too must the immune system. The damage to the organism resulting from immune dysfunction could be every bit as calamitous as that to the nation if its military organization failed. Put differently, the immune system is a double edged sword. Under ideal circumstances it diligently discriminates between self and non-self; selectively protecting, through the aegis of powerful biological weaponry against a plethora of pathogenic microorganisms and; like rooting out enemy infiltrators, it also guards against abnormal cell proliferation, eliminating malignant cells before they can multiply and corrupt the population.
Normally, the immune system performs efficiently and unnoticed by the host. However, in states of disarray, its effects are anything but unnoticed. Given the complexity of the system, as well as the fact that molecular similarities sometimes exist between self and foreign proteins, it is little wonder that on occasion it does fail. Failure might manifest in different ways. Over reaction to otherwise innocuous substances is termed allergy. The self destruction when the immune response is turned against the host, which is termed auto-immunity, can be devastating, as in multiple sclerosis, rheumatoid arthritis, myasthenia gravis, systemic lupus, and others. This would be similar to a military unit mistakenly attacking their own town folk.
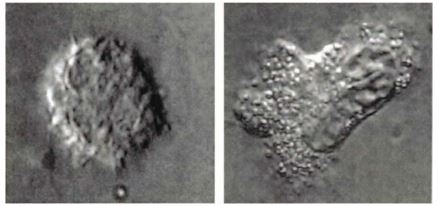
A prominent feature of innate immunity is the phagocytic cells. The killing mechanisms of phagocytes are very effective. They have been compared with infantry soldiers. In some respects they are actually more like kamikaze pilots. Phagocytes will engulf foreign pathogens into vacuoles then, merging with cytoplasmic granules containing highly toxic preformed proteolytic enzymes, destroy the pathogen. Like a kamikaze, they are usually destroyed in the process. In addition to these enzymes an activated phagocyte will also generate free radicals and other toxic reactive oxygen and nitrogen species. These can be taken up by nearby cells causing peroxidation of lipids in cell and organelle membranes, deformation of protein structures and damage to both nuclear and mitochondrial DNA.
It is noteworthy that overloading the macrophage/ monocyte system with the need to clear apoptotic neutrophils (i.e. dead kamikazes) allows some of them to undergo secondary necrosis, whereby uncleared cell fragments release their nucleosome fragments, which themselves may promote further inflammation and auto-immunity.(5) We often see that a commonly eaten food or food additive, will wipe out as much as 20% of the live neutrophils, in vitro, as determined by the Alcat Test method. This could well describe a model whereby food intolerance induces auto-immunity.
Interaction between the neutrophil and/or macro- phage and the invader is facilitated by the cell surface receptors’ ability to recognize molecular repeat structures on pathogen surfaces. Phagocytes also possess lectin receptors capable of recognizing mannose molecules on pathogens. However, many foods also contain lectin molecules and can easily be mistaken for pathogens, setting off a damaging response.
In some instances cells are assisted by the complement cascade of serum proteins, to effect binding of these markers on the pathogen surface, a process termed, opsonization. This occurs even on the very first exposure and is characteristic of innate immunity. Prior exposure is not necessary to initiate it and repeated exposure does not enhance it.
When bacteria with a polysaccharide capsule present, direct leukocyte contact is inhibited by the capsule. The ‘solution’ involves B-lymphocyte production of a specific antibody capable of recognizing a particular molecular structure, or epitope, associated with the micro-organism in order to facilitate binding. Phagocytes possess Fc ? receptors to facilitate this. Endocytosis and the further destructive sequence of events soon follow. This is characteristic of adaptive or, specific immunity as the antibody that is specific to the antigen (antibody generator) requires priming through prior exposure, and mounts a more efficient response upon re-exposure, as the formed antibodies increase their binding capacity as a result of affinity maturation.
When a virally infected or a cancerous cell, displaying altered surface markers presents, the altered cell will be destroyed by the direct killing action of a cytotoxic lymphocyte (CTL) or a natural killer (NK) cell.
If the host is attacked by a large pathogen, such as a parasite, other granulocytic cells (mast cells and basophils) release pre-formed histamine in a rather explosive fashion to attack the larger foe. This process is usually antibody mediated. Neutrophils may also react in this fashion toward a larger pathogen (or food macromolecule) in a process called frustrated phagocytosis.
Inappropriate activation, that is, reacting to a harmless substance such as a pollen grain as though it were a parasite, is termed allergy. Failure of the surveillance and neutralization of cancerous cells can result in neoplastic growth. Excessive generation of free radicals and reactive oxygen (and nitrogen species) and proteolytic enzymes, let’s call this intolerance, results in chronic inflammation, tissue and DNA damage, and leads to premature aging and possibly cancer. Inappropriate activation of CTL, and other defense mechanisms, aimed at self proteins, induces auto-immunity.
These imbalances, as well as simple nutritional strategies to redress them, will be examined in this review. As these responses are organism specific and involve cellular and molecular mechanisms, a practical cellular laboratory technique for determination of offending dietary factors to be avoided, the Alcat Test can be quite useful. The Alcat Test is a novel method for assessing cellular response to antigenic challenge, ex vivo, in whole blood that is exposed to a battery of test substances. It has demonstrated not only a benefit response to individually structured elimination of foods, but is also unique in that it exhibits a high correlation with double blind oral challenges with foods and food additives.
Allergy
The concept of allergy was fairly well understood when first introduce by von Pirquet, an Austrian physician, in 1906. It was intended to denote an altered reaction to a normally innocuous substance. As a matter of convention, Allergists later narrowed the definition of allergy to denote only such altered reactions that exhibit immediate and pronounced symptom onset.
It has been estimated that approximately 20% of the US population suffers from this form of allergy, also known as atopy, but this number seems to be growing rapidly. Reports suggest that as much as 54% of the population will show a positive skin test to at least one allergen. This is mainly in reaction to inhalant allergens, such as pollens, mites, and epidermals; occasionally some foods; peanuts and crustaceans being the most common, as well as some contactants. However, “true”food allergy, also known as classical food allergy; or a Gell and Coombs Type I reaction, rarely occurs, affecting less than 5% of the general population in the US.
Other reactions to foods and chemicals, reactions termed intolerances or sensitivities, where symptom onset is delayed and typically less acute in nature, occur considerably more often. Physicians distinguish between immediate allergic reactions, and adverse or toxic type altered reactions; referring to the latter as, “intolerance”, “sensitivity” or, “hidden” food allergies. Although both involve abnormal immune reactivity, the mechanisms underlying each differ from one another. Broadly speaking, classical allergy is a function of the specific immune system while, intolerance or sensitivity, primarily involves the innate branch of the immune system.
Classical Allergy is a Function of Specific Immunity
The hallmark of specific immunity is memory; hence the rationale underlying vaccine immunizations. It is specific in that it makes use of pathogen or allergen-specific binding sites on immunoglobulins (Ig) and lymphocyte receptors in the process of recognition. Prior exposure to the activating substance is necessary in order to elicit a response. Re-exposure induces a response more rapidly and with greater efficiency, as affinity maturation, better antigen binding, occurs.
As early as 1920, American allergists Praustnitz and Kustner demonstrated that passive transfer of allergy may occur by injecting allergic serum into the skin of a non-allergic subject. In attempting to discover the factor causing such allergic reactions they injected allergic serum into the subcutaneous tissue of the arm of a non-allergic. Subsequent scratch testing at the injection site with specific allergen induced a characteristic allergic wheal and flare. Although unknown at the time, the causative serum factor was referred to as reagin.
Immunoglobulin E (IgE)
In 1967 two independent teams of investigators identified reagin as the rarest of the five basic antibody isotypes, IgE. One team comprising a husband and wife in Colorado named Ishizaka. The other, at the Karolinska Institute in Sweden, later developed an immunoassay for quantification of allergen specific IgE- the RAST, an acronym for Radio Allergo Sorbent Test, a sandwich immunoassay using a radio- labeled anti-IgE antibody tag, read with a gamma counter.
The role of IgE in the pathogenesis of allergy was later elucidated. An antigen capturing and presenting cell (usually a macrophage or dendritic cell) takes up the allergen and degrades it. It binds to a major histocompatibility complex molecule (MHC molecule) and the MHC/allergen complex then migrates to the cell surface membrane. (All somatic, nucleated, human cells express MHC molecules for recognition of, “self” tissue.) MHC class II molecules present allergens or pathogen components to CD4+ (Cell Determinate) lymphocytes. A T-Helper 2 (i.e., lymphocytes that mature in the thymus gland) lymphocyte, with a conforming receptor will recognize the antigen pep- tide/MHC complex. Activation of the T cell requires not only this interaction, but also a co-stimulatory signal, usually involving a B7 molecule on the APC, and a CD 28 receptor on the T-cell. The T-cells, once activated proceed to chemically “instruct” those few B-lymphocytes that also possess surface receptors conforming to the initiating allergen peptide sequence.
In this allergic pathway the chemical message from the T cell to the B cell is Interleukin 4 (IL4). Activated B-cells mature into plasmacytes, efficient antibody producing factories, and continue churning out thousands of antibody molecules specific to the initiating allergen peptides. These cells then clone themselves as rapidly as their genetic machinery and availability of nutrients will allow. Each new cell is now also secreting soluble forms of the specific receptor molecule; allergen specific IgE antibodies, conforming to the peptide structures of the initiating allergen. The T and B lymphocytes that persist in the circulation following the resolution of an infection (or, as in this case, allergenic exposure) are termed memory cells.
T and B cells are notably allergen or pathogen-specific in so far as their recognition mechanisms are concerned. Hence, there will be relatively few memory T and B cells that initially recognize the specific antigen; however, those that do are capable of cloning themselves as rapidly as the cell’s genetic machinery and nutritional stores will allow upon repeated encounter with the pathogen. The key here is that the cells will require the appropriate signals (information) as well as the necessary store of nutrients to supply the needed building materials, as well as the enzymatic activity required by the synthesizing processes.
It is this capability of the memory cells to replicate and carry out their individual functions that underlies the human organism’s ability to counter a subsequent invasion by a particular pathogen much more rapidly than the 7 to 14 days required to gear up following the initial infection. Of course, this is a good thing when it occurs at the appropriate time; but, considering that common allergens, such as pollen grains, do not have the ability to multiply inside the body and, therefore, do not inherently possess significant potential for harm, allergy, per se, would have to be regarded as an inappropriate and itself harmful altered reaction. It can even be fatal at times, i.e., anaphylactic shock. The prevalence of allergy as well as that of intolerance is increasing and should be taken seriously.
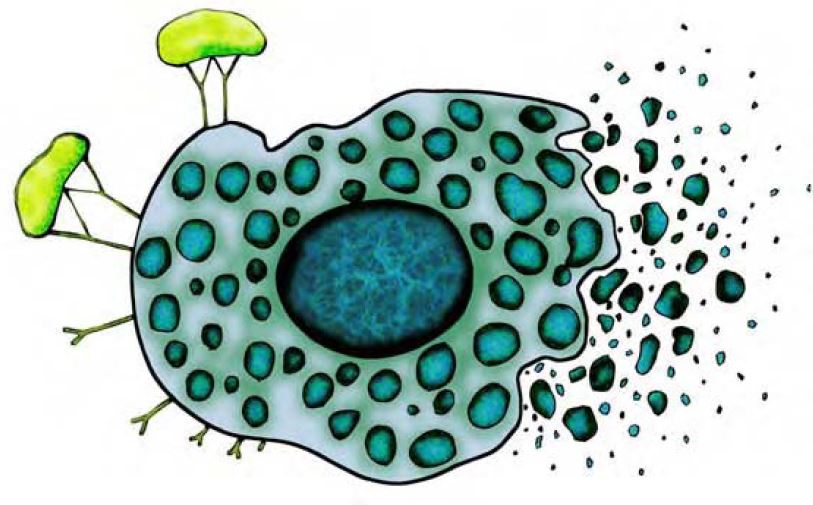
Once in circulation, IgE antibodies bind to surface fc receptors on mast cells in the connective tissue of the skin and mucosal linings of the respiratory, GI and genital-urinary tract; as well as with basophils in the circulation. These cells possess internal pre-formed mediator-containing granules, including histamine. When two or more cell-bound IgE antibodies subsequently encounter the specific allergen, their binding and “cross-linking” induces aggregation of cell membrane receptors, activating various enzymes and kinases, which in turn activate gene activation factors, such as NF?B, resulting in the release of these mediators, a process is known as degranulation (Figure 1). Inflammatory processes, including: increased blood vessel permeability, mucus secretion, irritation of nerve endings, and smooth muscle constriction – all common traits of “true” allergy, soon follow. The so-called late phase reaction, mediated by newly formed lipid mediators, products of arachidonic acid metabolism; leukotrienes, through the lipoxygenase pathway, and prostaglandins through the cyclo-oxygenase path- way, perpetuates the reaction and underlie what is referred to as the late phase.
The elucidation of this pathway is defined, and almost always involves IgE; thus, the RAST test can be quite useful in identifying these allergen triggers. However, as intolerance to foods or chemicals does not follow this pathway, RAST is of little benefit in identifying offending intolerogenic foods or ingested chemicals. Further, because IgE mediated symptom onset is rapid and dramatic, “true” allergic reactions to foods are usually obvious from the history thus obviating the need for testing. Intolerances to foods often produce delayed and less dramatic symptoms and are therefore less obvious.
Figure 1. When two or more cell-bound IgE antibodies encounter the specific allergen, their binding and “cross-linking” induces a process known as degranulation.
Many “allergic conditions” that involve the immune system do not involve IgE antibodies. Recently, investigators from the University of Rome found that chronic fatigue patients had significantly higher levels of eosinophil cationic protein than did controls (18.0 +/- 11.3 micrograms/l vs. 7.3 +/- 2.1 micro- grams/l (p?0.01) yet, this was not related in a significant way to allergen specific IgE levels.(6)
Dermatologists from Humboldt University in Berlin previously reported that urticaria patients respond favorably to elimination diets, particularly to elimination of pureed tomato products, and exhibited recurrence of symptoms upon double blinded oral challenge, independently of the presence of IgE recptors.(7)
Dr. Lene H?j from Denmark also reported on a study of patients with chronic urticaria (CU), as well as angioedema (AE), that were tested for reactivity to both foods and airborne allergens using RAST to determine levels of allergen specific IgE, total IgE, and 100 common foods, using the Alcat Test. A test outcome driven elimination diet modification produced a positive outcome in 45 out of 51 of AE. “High clinical significance also at long-term follow-up was obtained in severe AE and CU by applying results of Alcat Test, whereas IgE-mediated allergy played a minor role.”(8)
For this reason a lab test that can accurately identify offending foods and other environmental triggers, regardless of what the underlying mechanism may be, would be an invaluable tool for managing inflammatory conditions and would also trim health care costs. The Alcat Test is such a test.
In addition to the release of pre-formed mediators, particularly histamine, the cells will also synthesize prostaglandins, through the cyclo-oxygenase pathway, and leukotrienes, through the lipoxygenase pathway, which augment and prolong the reaction. Some leukotrienes can exert a constrictive effect on smooth muscles surrounding the bronchial tube many times more powerfully than histamine. The substrates of these pro-inflammatory lipid mediators derive from n6 fats which are incorporated into the phospholipids membrane, stored in peroxisomes in the cell, or, are present in the circulation.
At some point along the pathway of both n6 and n3 PUFA metabolism, competition exists for the same desaturation enzyme (? 5 desaturase). The n3 metabolites, in contrast to n6 metabolites, exert an anti-inflammatory effect. It is believed that during pre-industrial times the ratio of n3:n6 fats in the diet were in balance; something like a one to one balance ratio. Today, the standard American diet emphasizes consumption of the pro-inflammatory n6 substrates, products like corn oil, safflower oil, and rapeseed oil, also known as Canola oil, with a ratio of perhaps 20:1 Hence, dietary emphasis on fish oil consumption, to redress that imbalance, even more so than other foods containing n3’s, has been shown, in several studies, to have some effect on moderating the inflammatory processes. Consumption of high amounts of fish oils can significantly alter the cell membrane composition by perhaps as much as 15%, thus diminishing the available substrate for pro-inflammatory mediator production.
Both pre-formed and newly synthesized lipid mediators, as well as other cytokines, including, IL3, IL5, and granulocyte macrophage-colony stimulating factor, attract inflammatory cells, primarily basophils and eosinophils, but not neutrophils, to the local site of the reaction. A chronic state of inflammation and allergic lesions may ensue. Although neutrophils are not directly involved in Type I allergy, they do, as we’ll see, play a central role in intolerance reactions.
It is noteworthy that this pathway not only depends on the binding of the cell bound IgE antibodies with specific allergen, but also on a secondary or co-stimulatory signal by the antigen presenting cell. In fact in the absence of this secondary signal the T-cell may undergo apoptosis or become anergic (unresponsive) to the specific antigen. Anergy is an important mechanism by which T-cells develop tolerance to self proteins whilst they are maturing in the thymus. That is, T cells, while maturing, if exposed to self proteins, will either become anergic; or, if reactive, apoptotic. A breakdown of this mechanism is likely to result in auto-immunity.
Therefore, claims that an in vitro lab test will detect either allergy, or intolerance, when a specific condition of the assay calls for the isolation of the lymphocytes in autologous serum (because; by definition, the antigen presenting cells and the necessary co-stimulatory signal they provide are absent), should be taken with skepticism. This is the case with the “ELISA-ACT Test” which neither has a sound scientific basis nor has ever been validated by comparing it to the “Gold Standard”, a double blind oral challenge, because the promoters believe that no such standard exists.(9)
A useful lymphocyte proliferation assay should either be carried out on whole blood, where the normal cell to cell interactions are preserved, and growth factors are present; or, the sample should be enriched with macrophages or monocytes, to perform the role of antigen processing and presentation.
Modulation of the Specific Immune Response to Prevent Allergy
Thus there is clear evidence that IgE triggers allergy. A therapeutic strategy of injecting antibodies targeted against the cell binding (fab) portion of the IgE molecules appear to block the interaction at a critical point and thus prevents mast cell and basophil activation. In some test subjects, allergic subjects appear to have achieved tolerance to peanut under experimental conditions. However, there can be an untoward side effect of down regulating IgE, notably, compromising parasite defenses.
As the T-Helper 2 pathway is activated by parasitic infections the resulting explosive release of histamine is effective when confronting a pathogen of such relatively large size. Thus, non-specific blocking of the IgE mechanism may render the organism more susceptible to this form of infection.
A more specific therapy has been researched which, theoretically, will block a specific allergen reaction while leaving the general protective function of the immune system intact. This approach to classical allergy therapy lies with redirecting or modulation of this pathway to the non-allergy provoking T Helper 1 pathway.
When challenged with a viral or bacterial antigen instead of a parasite, T Helper 1, as opposed to TH 2 cell differentiation, is induced and the signals transmitted to B cells, notably, ? interferon (as opposed to IL 4), induces isotype switching to IgG, rather than the pathogenic IgE isotype. Instead of binding to mast cells and basophils and inducing them to release their deadly chemical arsenals, IgG antibodies, which are about 10,000 times more prevalent than IgE, opsonize the pathogen, enabling phagocytic binding and blocking of the pathogenic IgE antibodies.
This therapeutic effect is achieved by the use of injections of “immunostimulatory sequences” (ISS) of bacterial or viral nucleotides, covalently bound to the specific antigenic epitope. The bacterial or viral nucleotides induce a TH1 rather than the TH2 type response. Promising clinical results have been obtained using the specific allergenic epitope of ragweed pollen, Amb a 1, which will activate a TH 1 cell with a receptor molecule specific to that antigenic epitope. In this way, the non-allergy provoking TH1 response to the specific allergen is up-regulated, in direct proportion to the subsidence of the allergenic TH2 pathway.(10)
Hence, the reaction leads to the production of allergen specific IgG antibodies. In this fashion non allergy provoking, ragweed allergen specific IgG blocking antibodies are produced rather than the reaginic allergy provoking IgE antibodies.
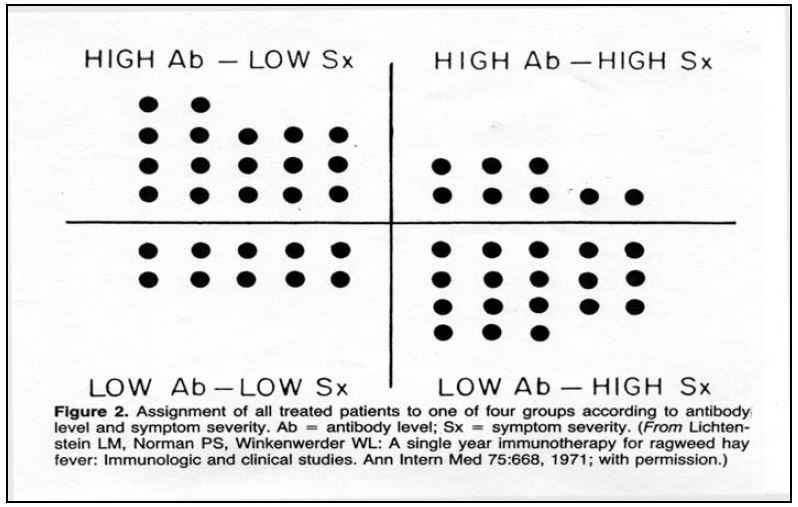
Figure 2. As immunotherapy for atopic allergy progresses allergen specific IgE antibody titers decline while allergen specific IgG antibodies increase.
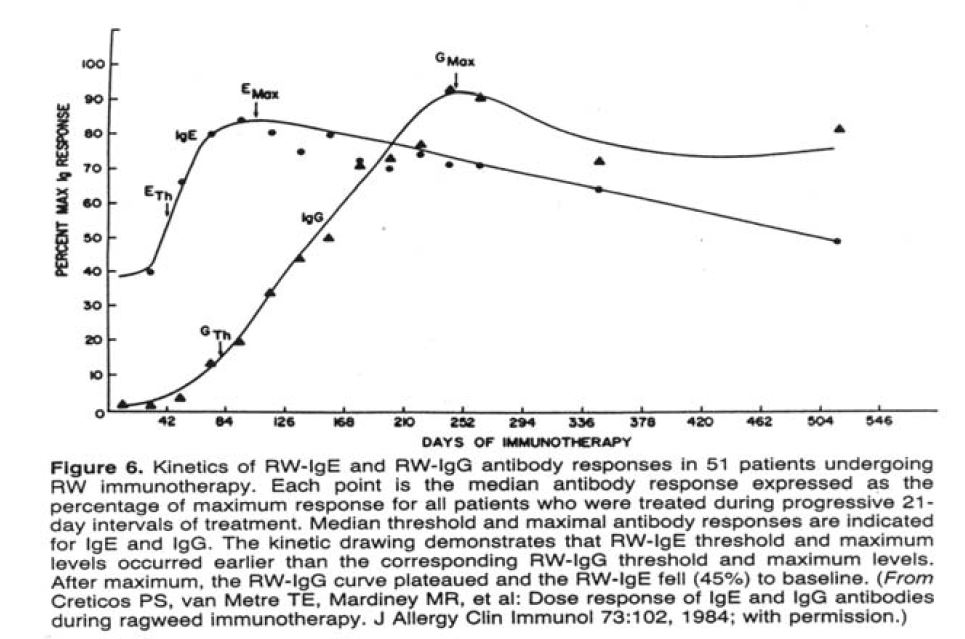
The Protective Role of IgG
Frequent and high exposure to an antigen favors an IgG response, whereas low level and infrequent allergen exposure induces an IgE response. Herein lays the rationale underlying classical immunotherapy vaccines, referred to as “allergy shots”, in use since 1911. The theory is born out by studies showing that as immunotherapy treatment for classical allergy progresses, allergen specific IgE titers decline, while titers of specific IgG increase (Figure 2). As the IgG increases, symptoms also abate (Figure 3). IgG is not an allergy provoking antibody; as in the case of viral or bacterial infection, it is protective.
Figure 3. As allergen specific IgG antibody titers increase, symptoms decline.
Just as IgG is not allergy provoking, a number of studies have also shown that IgG does not cause food intolerance related symptoms:
- In their 1999 paper Keller et al write: “the occurrence of IgG-cow’s milk antibodies is a physiologic phenomenon without diagnostic significance.”(11)
- Hadjivassiliou et al conclude: “IgG anti-gliadin antibodies have a high sensitivity not only for patients with celiac disease, but also for those with minimal or no damage…When the histological criteria of celiac disease are used as the gold standard IgG, anti-gliadin antibody has low.” (12)
- In their paper entitled“Allergenicity of major cow’s milk and peanut proteins determined by IgE and IgG immunoblotting”Szabó and Eigenmann write: “The presence of IgG antibodies in non-allergics was related to regular ingestion of ”(13)
- Jenkins and Vickers reported: “We found no evi dence that IgE/IgG4 antibody test…is a reliable diagnostic ” (14)
- Zar, Kumar, and Benson sum up the situation in their paper, Food hypersensitivity and Irritable bowel Syndrome (IBS): “In fact, several studies have suggested that IgG and IgG4 production may be a normal immunological response to dietary antigens is probable that food hypersensitivity is a heterogeneous condition, and that more than one immunological abnormality may exist.”15
IgG maintains its protective role with respect to excess food antigens in the circulation by complexing with them and assisting the monocyte-macrophage system in their elimination; without inducing pathology. High IgG titers correlate with exposure, not sensitivity. Hence, allergen specific IgG testing is not of accurate in assessing food intolerance.
Thus, this specific branch of the immune system provides protection against specific foreign pathogens. It requires prior exposure to the pathogen in order to mount a targeted and specific response. Misidentification of normally non-pathogenic substances, such as pollens, mite feces, drugs, epidermals, and (occasionally) foods and other factors may induce an altered reaction, or allergy. Allergic reaction is very much a function of the specific immune system; it produces distinct symptomology and it follows a well defi and clearly understood pathway. Food intolerance, on the other hand, is induced by multiple pathogenic pathways – some immune and some non-immune, induces chronic and less acute symptomology, is not IgG related, is both genetically determined yet exposure related; and therefore is far less well understood and consequently, under-treated.
Innate Immunity
Despite the lack of supporting scientific evidence many labs promote allergen specific IgG testing for food intolerance. Confusing as it, the role of IgG in the pathology of food intolerance causes many clinicians, unsurprisingly, to misconceive that prior exposure to a food is necessary in order to develop sensitivity to that food, as indeed it would if food intolerance were a function of specific immunity. For instance, the late Robert Atkins of low-carbohydrate diet fame once questioned the author as to why all of his kosher pediatric patients were testing positive to pork on the Alcat Test, when, by definition none of these patients had a prior exposure. A reasonable viewpoint if in fact food intolerance were a function of specific immunity. However, it is not. Rather, food intolerance is primarily a function of innate immunity.
Innate immunity may be activated by various factors, and priming, or previous exposure, is not a pre-requisite. As Dr. Charles A Janeway, Jr., Professor of Immunobiology at Yale states, “The innate immune system is born with the ability to recognize certain microbes…(and) can destroy many pathogens on fi encounter.” (How the immune system recognizes invaders, Scientific American, Sept. 1993) The innate immune system also has an inborn ability to recognize offending foods.
The complement system, a major component of innate immunity, is a cascade of serum proteins first described by the Belgian bacteriologist, Jules Bordet in 1900. These proteins “complement” the activity of antibodies to opsonize the membranes of microorganisms, thereby facilitating phagocytosis. Complement proteins are non-specific; they will bind indiscriminately. However, host cells secrete enzymes that normally inactivate complement; an example of self /non-self discrimination.
The complement system also protects from detrimental microorganisms by attaching to their lipid membranes and assembling various components of the cascade called the membrane attack complex. This involves components C5 through C9, unimagi- natively named in order of their discovery. They are capable of puncturing the membrane, thereby causing the inward rush of surrounding fluid and resultant destruction of the invader.
Some microbes, such as those causing pneumonia or streptococcus infections, wear a polysaccharide coat in an attempt to block the attachment of the complement proteins. This is dealt with in one of two ways: either the tissue macrophages, which have receptors for these sugars, can bind directly to the bacteria; or, the activated macrophage will release interleukin 6 inducing hepatic production of mannose binding protein, which will itself bind the bacterium, and then activate the complement cascade.
As mentioned, excess antigen is cleared from the circulation by complexing with IgG antibodies. Sometimes, a Gell and Coombs Type III immune reaction, also known as immune complex disease, may occur wherein immune complexes are deposited in tissue or joints and attract inflammatory cells to the site, as in rheumatoid arthritis and glomerulonephritis. But, these are usually IgM antibodies rather than IgG. In examining 1012 renal biopsies from patients with glomerulonephritis through electron microscopy, Dr. M Haas from the Department of Pathology at Johns Hopkins School of Medicine observed that such immune complexes were comprised of antibodies of the IgM isotype, and rarely of IgG. However the predominant component was C3, a key component of the complement cascade.
These findings are consistent with what researchers found while investigating the various mechanisms involved in food-induced asthmatic reactions (Figure 4). When the blood of nine asthmatic patients was analyzed to food reactions as measured by the Alcat Test, and compared to double- blinded oral challenge, there was a high level of correlation observed. Other immune parameters were measured. High correlation was also seen with activation of the complement cascade. Significant changes pre and post in vitro food challenges were also seen in levels of IgM antibodies, but not IgG antibodies. IgG antibodies do not appear to play a significant role in food sensitivity and are likely to be protective in that they block reaginic antibody action and facilitate natural clearance of excess antigen from the circulation without provoking symptoms. The cellular reactions (changes in cell size and/or count following in vitro challenge) seen by the Alcat Test, do appear to be clinically relevant and reflect multitude of pathogenic mechanisms, often associated with complement activation.
Figure 4. Multiple pathogenic mechanisms in food sensitivity reaction in vitro.
The most common phagocytic cells of the innate immune system are the neutrophils. These are the one class of granulocytes that are not involved in the late phase reaction of type I allergy; however, they usually comprise more than 90-95% of the granulocytes in circulation. The overall system is an effective first line of defense in acute infection but chronic activation leads to disease. Unlike T or B cells, they have a short half life and are very aggressive.
As mentioned earlier, neutrophils destroy pathogens in various ways, but predominantly by generating highly toxic reactive oxygen and nitrogen species, and/or releasing powerful proteolytic enzymes. These include, superoxide anion, which will react with the neutrophil mediator, myeloperoxidase to form hypochlorous acid; peroxynitrate; hydrogenperoxide – which is not a free radical but is still highly toxic, and others.
Figure 5. When neutrophils become activated they release toxic mediators of inflammation as well as reactive oxygen and nitrogen species, these are damaging to pathogens but also damaging to host molecules and tissues.
Inflammation and Oxidative Stress
This is where we see the link between chronic activation of the innate immune system and the degeneration described in Denham Harmon’s free radical theory of aging.
William R Clark, Professor Emeritus of Immunology (UCLA) describes some of the effects of neutrophil activation in his book, A Means to an End: The Biological Basis of Aging, Oxford University Press, 1999: “One of the more common sources of reactive oxygen species in the body as a whole is from cells that use the destructive power of these molecules as a natural defense against microbial infection. Phagocytes (literally, “eaters of cells”) such as macrophages and neutrophils, purposely generate high levels of oxygen radicals, which they store in tightly sealed intracellular compartments…. Oxygen radicals released in this fashion can be taken up be adjacent cells, and once inside they cause the same sort of damage as radicals produced internally….in the case of prolonged infections a chronic inflammatory state may develop, and the repeated engorging and death of phagocytes can cause serious oxidative damage to nearby healthy cells. This is also a major source of damage in chronic inflammatory autoimmune reactions such as rheumatoid arthritis, and can lead to serious tissue loss.
The damage done by reactive oxygen molecules needed to operate living cells can be enormous. No molecular species is immune. Oxygen radicals can attack and deform proteins molecules, disrupting structural complexes and inhibiting important enzymatic functions….Oxygen radicals also attack the individual nucleotide bases that make up both nuclear and mitochondrial DNA.”
The Free
In 1956 Denham Harmon proposed “The free radical theory of aging” in which he postulates that random deleterious tissue damage results from the generation of reactive oxygen species (ROS) and nitrogen species (RNS). Subsequent observational studies have lent support to this theory. As tissue deteriorates with age there may be a general increase in the level of ROS and RNS production. Of note is that aged rat mitochondria produce more superoxide anion than that of young rats suggesting ‘leakier’ electron transport and the ensuing mitochondrial damage. It is suspected that other ROS and RNS also exhibit increased production in other tissue as a function of age.
Further evidence of increased free radical activity and aging comes from the observation that larger animals consume less oxygen per unit of body mass than do smaller animals and exhibit a correspondingly longer lifespan. Similarly, cold blooded animals are more resistant to oxidative stress when maintaining a lower body temperature. Presumably, lower metabolic activity produces fewer free radicals and other ROS. Decreasing the flying activity of drosophilae by wing clipping or space restriction markedly increases survival time. Similarly, Queen Bees, which do not fly, live approximately 50 times longer than the worker bees that do.
Wolford has presented compelling evidence that caloric intake, which lowers metabolism and free radical production, is associated with increased lifespan across a range of species, including primates.
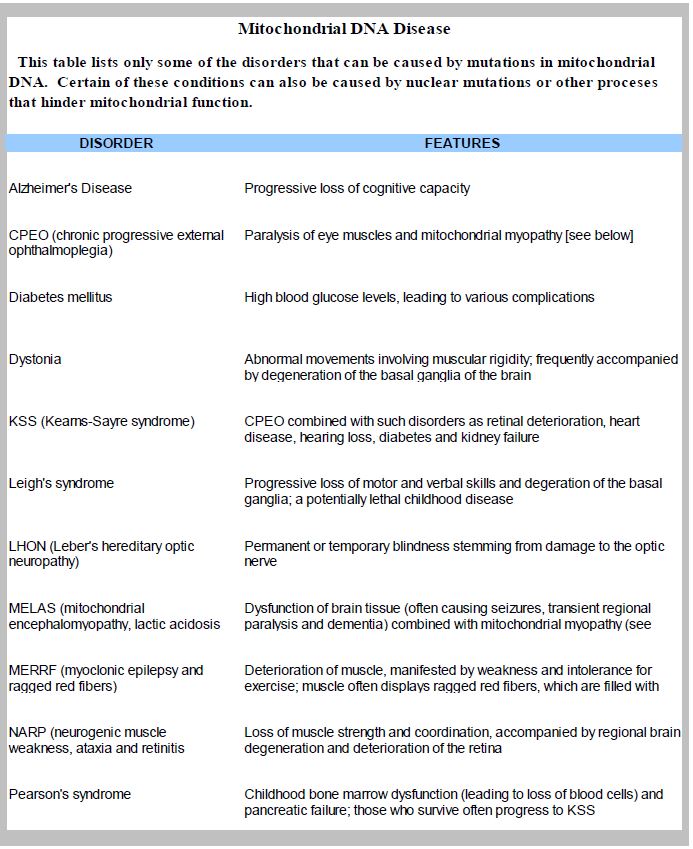
Table 1. Diseases associated with mitochondrial DNA mutations.
The bulk of aerobic metabolism, and, therefore, oxygen consumption, occurs in the mitochondria. Hence, higher levels of damage occur to DNA in mitochondria, especially deletions, as compared to nuclear DNA. This is indicated by levels of 8-hy- droxy-deoxyguanasine, observed in human brain, liver, and other tissues. It increases with age and produces a decline in the function of mitochondrion and the cells they provide energy to. A number of disorders are associated with mitochondrial damage (see Table 1).
Chronic Inflammation and Degenerative Disease
Many investigators have documented the role of neutrophil mediated inflammatory processes in a range of degenerative diseases. Crocker et al reported that peripheral blood neutrophils of pre-eclamptic woman are significantly more responsive to the agonists zymosan and fMLP, in terms of free radical production and the upregulation of other markers of cell activation, than are the cells of women with normal pregnancies or age-matched controls.(16) The authors conclude: “Circulating neutrophils are neither activated nor primed in vivo, however the re- lease of reactive oxygen species is diminished in normal pregnancy. In comparison, an elevation of reactive oxygen generation in preeclampsia may highlight a role for neutrophils in the oxidative stress and pathology of this disease.” There are also anecdotal reports of previously infertile women becoming pregnant after following an Alcat Test directed diet for a few months.
Rheumatoid arthritis is clearly an inflammatory condition. Investigators from New Zealand reported a two to eight fold increase in phagocytic (neutrophils and monocytes) free radical production versus that of non-rheumatics and healthy controls. Notably, the increased levels of superoxide production seen in the rheumatic subjects correlated well with TNF-alpha, but there was no correlation with plasma levels of C-reactive protein and only slight correlation with erythrocyte sedimentation rate (ESR).(17)
Recently, investigators from Harvard observed that neutrophils of poorly managed diabetics released significantly higher levels of free radicals following stimulation than did those of patients whose blood sugar levels were well managed or normal controls.
They also observed a significant correlation with blood sugar levels and severity of periodontal disease and postulated that high blood sugar levels induce priming of neutrophils.(18)
Inflammation is increasingly being seen to be at the source of a diverse range of degenerative diseases. The authors conclude that, “Inflammation and oxidative stress are important factors in the pathogenesis of diabetes and contribute to the pathogenesis of diabetic conditions.”
Research has shown that when neutrophils adhere to cardiac myocytes the latter incur significant damage via the NADPH oxidase enzyme system mediated oxidative burst. Researchers from the Immunology Research Group at the University of Calgary investigated the role of the adhesion molecule alpha (4) integrin. They observed that neutrophils that left the circulation and adhered to cardiac myocytes quickly induce myocyte shortening by 30-50% and rates of contraction and relaxation by 30%, within the first ten minutes. Furthermore: “An increased level of oxidative stress was detected in myocytes within 5 min of PMN (polymorphonuculear cells) adhesions.” This effect was blocked by anti- alpha (4) integrin antibodies and also by extracellular superoxide dis- mutase (SOD) suggesting superoxide anion as the effector mechanism. The authors conclude: “The results also provide pathological relevance as the emigrated PMN’s have the capacity to injure cardiac myocytes through the alpha (4) integrin-coupled NADPH oxidase pathway that can be inhibited by extracellular, but not intracellular SOD.”(19)
One of the most frightening of age-related diseases (for those who are aware of it) is cognitive decline. Proving once again what the legendary Indiana Jones stated to his much younger girlfriend: “It’s not the years, it’s the mileage!” French researches at the laboratory of Immunology (INSERM) investigating the role of neutrophil induced oxidative stress in Alzheimer’s and Parkinson’s patients, have indeed shown that levels of oxidative stress, and not chronological age, are most relevant to these conditions: “As circulating neutrophils are the most powerful sources of reactive oxygen species, we measured oxidative stress levels in resting neutrophils from 44 Alzheimer’s and Parkinson’s disease patients and compared them to 40 healthy counterparts. Significantly increased oxidative stress levels were observed in patient’s groups while control groups had very similar levels irrespective of age.” They conclude, “Our results indicate that oxidative stress levels in circulating neutrophils are of interest for further mechanistic studies of neurodegenerative diseases and might open the perspective of a diagnostic tool.”(20) Indeed, the Alcat Test is such a diagnostic tool, as it measures the activation of circulating neutrophils when exposed to common foods and other environmental factors.
Atherosclerosis is the end point of an inflammatory process occurring within the intima of the artery mediated by chronic immune system activation. It occurs when oxidized cholesterol becomes a factor in the formation of plaque. As the oxidized cholesterol is consumed by macrophages they convert to foam cells. The result is stenosis of the artery, laying the basis for a stroke following a thrombotic event.
Investigators from Humboldt University in Berlin have measured plasma levels of fragments of the cell membrane lipid, phosphatidylcholine (PC) in blood plasma by HPLC and found significantly higher concentrations of PC in elderly coronary heart patients than in young healthy controls. Elevated fragmented PC was also seen following the smoking of even one cigarette and also during the reperfusion period following bypass surgery, which coincided with a surge in circulating neutrophils. These investigators also observed elevated PC levels in vitamin E deficient rats and concluded that plasma PC fragment levels increase following various forms of oxidative stress. Of course, fragmented cell membrane lipids may be metabolized to inflammatory eicosanoids.(21)
Dr. R Zhang and co-investigators reported in the Journal of the American Medical Association in November 2001, Association between myeloper- oxidase levels and risk of coronary artery disease, a significant association between both blood and leukocyte levels of the neutrophil produced inflammatory mediator, myeloperoxidase (MPO) and the presence of coronary artery disease (CAD). They concluded: “These findings support a potential role for MPO as an inflammatory marker in CAD and may have implications for atherosclerosis diagnosis and risk assessment.”(22)
Another group from Shandong University very recently reported on the significance of MPO in cardiovascular disease by demonstrating a possible role for this neutrophil produced inflammatory mediator in the oxidation of low density lipoproteins. Referring to measurements of MPO and high sensitivity C-reactive protein in both cardiovascular patients and controls they find, “MPO is a better marker for inflammation of local plaques. It may be one of the mechanisms that MPO induces the transforming from LDL to ox-LDL in plagues vulnerability.”(23)
Also, In 2001, Duncan and Schmidt performed a meta analysis of the association of infl tory markers of the innate immune system and diabetes, cardiovascular disease, and obesity. Their analysis revealed “…evidence to suggest that chronic activation of the innate immune system may underlie the metabolic syndrome, characterizing the common soil for the causality of type 2 diabetes mellitus and cardiovascular disease.” They conclude: “Better understanding of the role of the innate immune system in these diseases may lead to important advances in the prediction and management of diabetes and cardiovascular disease.”(24)
Similarly, obesity is a complicated and frustrating problem involving neurological and endocrine as well as immunologic components. In a study performed at Baylor Medical College, Sports Medicine and Performance Institute in Houston, reported in The Bariatrician, Spring 1996, entitled, The Short term efficacy of the Alcat Test of food sensitivities to facilitate changes in body composition and self-reported disease symptoms: a randomized controlled study, it was found that overweight subjects fol- lowing an eating plan eliminating foods suspected of activating innate immunity, based on laboratory analysis of whole blood samples, experienced a significant improvement in body composition and scale weight.
The effect of immune activating foods was distinct from that of caloric restriction, as a well matched control group that followed a calorie restricted diet was included in the study. The report, by Gilbert Kaats, PhD and co-workers states that “80 percent of the subjects in the experimental group lowered their body fat during the study compared to 34 percent in the control group. 78 percent of the experimental group achieved an improvement in their body composition compared to 29 percent in the control group… and 98 percent of the subjects following the Alcat Test plan either lost scale weight or improved their body composition.
Professor Cabo-Soler, Chief of Biochemistry at the University of Valencia reported in 1995 that iso-caloric food elimination diets, based on Alcat Test results, promoted enhanced weight loss, comprised more of adipose tissue, rather than muscle mass, as determined by DEXA studies.
One plausible interpretation of these data is that altered immune system reactions to the preponderance of artificial, genetically novel foods, and other environmental challenges, may overwhelm Phase I and Phase II detoxification capacity, thus triggering chronic innate immune activation. This, to a great extent, may account for the dramatic increase in metabolic syndrome and other chronic degenerative disorders seen in industrial societies. The lower nutritional value of commercially produced agricultural products is likely also a contributory factor.
Possible Causes of Food Sensitivity
It appears that multiple mechanisms are involved in adverse reactions to foods. An enzyme deficiency, such as a lactase deficiency may manifest lactose intolerance. Whilst additives used in prepared foods have been found to be particularly problematic. Professor Brostoff, from the Middlesex Hospital Medical School of the University of London explains that azo dyes, used extensively in prepared foods, will inhibit the activity of phenyl-sulpanotransferase-P, which breaks down cresol-P in the gut. If cresol-P is not broken down it may become neurotoxic. Benjam Feingold warned about food colorings in the 60’s with respect to hyperactivity in children. Results of a multi-disciplinary study of autistic children showed that all of the subjects had at least some reactivity to food colorings, as determined by our in vitro cellular assay.(26) Similarly, many foods contain chemicals, or have chemicals added to them, which are intolerogenic. Salicylates, for example, occur in many fruits and vegetables, and can induce a pharmacologically mediated adverse reaction in susceptible individuals.
Dietary lectins, which may be resistant to degradation through cooking and digestion, occur in numerous vegetables, fruits, grains, and some meats. All mammalian blood and tissue cells have membrane carbohydrate molecules that bind lectins and may cause reactivity. Some lectins can even bind to multiple fc receptors on mast cells, which triggers histamine release similar to that which is seen in classical allergic reactions. However, some lectin activity is actually benefit, in that it may augment the normal immune response. This, as well as some other lectin activity, is not blood type specific. There is no convincing scientific evidence that blood type is associated with specific food induced pathologies.
Recently, Dr. Lu Shan and co-investigators from multiple departments at Stanford University and the Institute of Immunology from the Rikshopitalet in Oslo, reported in a paper entitled, “Structural basis for gluten intolerance in celiac sprue“, identifying a 33- mer peptide, rich in proline and glutamine, which was highly resistant to gastric, pancreatic, and small intestinal brush border membrane proteases. They also found that it occurs in all grains that are toxic to celiac sprue patients (wheat, rye, oats, and barley) but is absent in other grains. Additionally, the peptide was shown to be a potent stimulator of T cells (CD+, or helper type) in 14 out of 14 celiac sprue patients. However, in both in vitro and in vivo assays the peptide could be broken down by bacteria derived prolyl endopeptidase (PREP), thus suggesting a possible treatment strategy.(25)
Similarly, many naturopathic physicians and others have maintained for years that a gut dysbiosis or a “leaky gut” whose failure to degrade food components, may be an inciting factor when undigested proteins traverse the gut prematurely and enter the circulation.
Synergism
This model illustrates an adverse reaction to foods, in this case gliadin fractions occurring in grains, that involves activation of specific immunity; the T cells of celiac patients with a specific leukocyte antigen which then release potent cytokines, attracting inflammatory cells of the innate immune system which cause damage to local tissue through the release of their toxic mediators.
An additional feedback loop from innate immune reactivity to specific immune function is observed when activation of the innate immune system up-regulates the expression of B7 molecules on antigen presenting cells, which, as seen in classical allergy, for example, provide the secondary signal necessary to turn on T helper cells. Thus, the coordination of the two branches of the immune system is suggestive of a complex synergistic function and it is often seen that treatment of allergy decreases food intolerance; and, conversely, the effective management of food intolerance, improves allergic states.
Nonetheless, classical allergy is mediated by the specific branch of the immune system and the broad category of adverse reactions to foods are mediated, primarily, by the innate branch of the immune system, secondary to gastrointestinal dysfunction and/or detoxification insufficiency. Although several factors can induce histamine release, usually it is IgE. Symptom onset is immediate and it requires a small dose of allergen to trigger symptoms.
Food Sensitivity is Multi-Factorial
Multiple pathogenic mechanisms are involved in ad- verse reactions to foods, some of which are immunologic; others, toxic or pharmacologic. Symptoms are typically dose dependent, and symptom onset is delayed.
Adverse reactions to foods are hard wired in our genes, but susceptibility is dependent upon many factors; such as the integrity of the natural barrier of the gut wall, the viability of phase I and phase II detoxification pathways, and the presence or absence of other co-factors. A combination of these conditions could push one over their level of tolerance at any given time. It should be borne in mind that the human lymphocyte possesses all of the enzymes and substrates that are involved in hepatic detoxification and therefore serves as a back up system, albeit, one that may provoke unwanted symptoms.
It is sometimes seen that reactions to apple do not occur unless airborne birch pollen, which cross reacts with apple, is high. A food which contains an intolerogenic chemical is tolerated in moderation; but over consumption of it, or it in combination with other food(s) dependent on the same detoxification pathway may overwhelm that pathway and produce symptoms when consumed on a more frequent basis. Therefore, nutritional status which supports detoxification can exert a significant impact on food intolerance states, thus meaning that rotational eating plans may be beneficial for food intolerant patients.
In exercised induced asthma, increased body temperature serves as a co-factor with antigen to induce the degranulation of basophils, and histamine release, not occurring at normal body temperature.
Stress produced cortisol will destroy secretory IgA antibodies in the gut (and at the site of other mucus membranes as well) allowing for the perfusion of undigested food macromolecules that may activate the immune system. Intestinal dysbioses, Type I allergy in the gut, prescribed cortisone, and other variables may also contribute to a leaky gut.
Given the complexity of food intolerance it is easy to appreciate the need for a rapid, cost effective and accurate laboratory test to substitute for the laborious process of elimination and challenge, which, if properly performed, would take months, and try the patience of even the most patient of patients, not to mention their health care provider.
Figure 6. The Alcat Test diagnostic system.
Laboratory Testing for Food Sensitivity
We began our development of a reliable test for food intolerance in 1984. Previously, during the 1930’s, allergists Cooke and Vaughn focused on changes in white blood cell counts following an in vivo challenge with a battery of foods. Initial successes encouraged others to continue this line of research utilizing microscopic observations of white cells following antigenic challenge in vitro. These methods offered some tantalizing results but were crude and results were not reproducible.
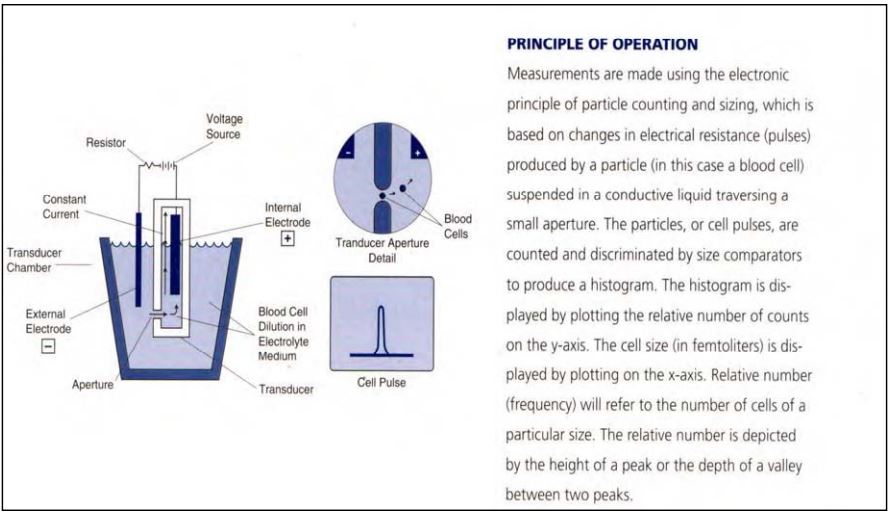
Our efforts focused on the utilization of electronic methods of cell measurement and computer analysis of the results following an ex vivo challenge of whole blood with food extracts and other substances suspected of association with non-IgE mediated hypersensitivity (Figure 7).
Analysis of whole blood offers a significant advantage in that it contains all of the immune factors, cellular elements and serum proteins that might be involved in an adverse reaction of this type, regardless of the underlying biological mechanism. Regardless of the various pathways that may underlie an adverse reaction to a food, the final common pathway will involve some mediator release. The cellular processes that occur; either swelling (vacuolization) decrease in number (destruction following degranulation) or shrinking (probably partial degranulation) are measurable through the Alcat Test.
Figure 7 . The principle of operation behind the Alcat Test.
It has been demonstrated by Mele et al from the Sacred Heart Catholic University of Rome that leukocytes which have reacted to Alcat Test positive food extracts in vitro, become incapable of releasing mediators when subsequently challenged by zymosan, an indication that the positive Alcat Test is associated with cell activation, and subsequent depletion of mediator stores.(28) Hence, a hypothesis that food intolerance reactions deplete immune resources and renders the subject more prone to infection, as has been observed, is not unreasonable. The method of measurement is the impedance or “Coulter” method that is used in routine hematology. It has demonstrated a high degree of correlation with clinical manifestations as confirmed through a rigorous double blind trial.
Drs. Peter Fell and Jonathon Brostoff reported an 83.4% correlation with Alcat Test results and double blind oral challenges with foods. (45th Annual Congress of the American College of Allergy and Immunology). Whilst Hoj et al reported a 96% correlation with Alcat Test results and double blind placebo controlled oral challenges with food additives.(27) (Journal of Allergy and Clinical Immunology, Vol.97 part 1, Jan., 1996). Hoj et al also reported a random sampling of clinical outcomes across a range of conditions suggesting the test results are accurate and useful in treating these conditions (Figure 8).
Figure 8. Results of an outcome study by Hoj et al, of patients following the Alcat diet plan.
Alcat Nutritional Assessment (ANA)
Professor Roger Williams, in his 1956 classic book, Biochemical Individuality, wrote: “Nutrition applied with due concern for genetic variations, which may be large, off the solution to many baffling health problems.”
The Alcat Test methodology can be adapted to perform a functional assessment of specific nutrient deficiencies. A functional test is superior to an assessment of levels of a specific nutrient in serum or other physical sample because an individual’s level may fall within a “normal” range, but may be inadequate for that particular individual due to a number of factors. Some of these factors are genetically determined while others are phenomenological; such as, impaired absorption, increased requirements due to stress (i.e. pregnancy, drug use, impaired transport through the blood secondary to inadequate protein binding molecule function, inadequate cell uptake secondary to cell membrane abnormality, inade- quate supply of co-factors) etc. Thus, serum tests may indicate normal levels, yet that particular individual, due to factors unique to them, is deficient.
Lymphocytes are metabolically active cells that are easily obtainable and reflect long term nutritional status, having an average life of approximately six to nine months. In this regard, measurement of nutrient impacted Lymphocyte growth and division will depict a more long term status, not one significantly impacted by vitamins or other supplements consumed just prior to testing. As such, this testing approach is analogous to how the measurement of Hemaglobin A1c represents long term (approx. 3 months) blood sugar balance.
Cell division and growth of lymphocytes represents metabolic pathways that are common to all reproducing cells and also indicates proficiency of immune system function. The lymphocytes that clone themselves to combat a specific pathogenic microorganism, at the time of infection, leave behind a few examples of their type as memory cells to get a head start on combating the same pathogen on subsequent exposure. The success of the secondary immune response will depend on how quickly those memory cells can proliferate and produce specific antibodies upon re-exposure to the pathogen. That rate of proliferation will be limited by the intracellular stores of nutrients needed for new DNA synthesis and cell growth. The Alcat Nutritional Assessment (ANA) is expected to indicate specific deficiencies that reflect the totality of cells but also those that are critical to the specific immune response.
The advantages of the ANA over other nutritional assays, even a cellular functional assay, is that testing whole blood preserves the normal cell to cell interactions and presence of the natural growth factors involved in cell division, and also eliminates a lot of cumbersome preparation procedures. It also allows for ease of measurement, avoids the requirement for radioactive material used in the old fashioned process of lymphocyte proliferation tests, and promises high accuracy, efficiency and reproducibility. The Alcat Test method of measurement of lymphocyte proliferation may also be applicable to other uses, such as determination of vaccine effi y (i.e. recall antigen induced proliferative response) and the monitoring of various immune proficiencies.
The assay will run on the current instrument platform with only minor software changes. Test kits can also be configured using the current Alcat Test kit cassettes.
Concluding Remarks
Measurement of immune function and response to dietary and other environmental factors using cellular laboratory assessment represents a viable and practical approach to optimization of immune function and normalization of the inflammatory response to the benefit of health and longevity.
Literature
- Harman Free radical involvement in aging. Pathophysiology and therapeutic implications. Drugs Aging. 1993;3:60-80. Re- view.
- Morris A forkhead in the road to longevity: the molecular ba- sis of lifespan becomes clearer. J Hypertens. 2005;23:1285-1309. Review.
- O’Connell PJ, Wang X, Leon-Ponte M, Griffiths C, Pingle SC, Ahern A novel form of immunesignaling revealed by trans- mission of the inflammatory mediator serotonin between den- dritic cells and T cells. Blood. 2006;107:1010-1017. Epub 2005 Oct 13.
- Kelley DS, Taylor PC, Nelson GJ, Schmidt PC, Ferretti A, Erickson KL, Yu R, Chandra RK, Mackey Docosahexaenoic acid inges- tion inhibits natural killer cell activity and production of inflam- matory mediators in young healthy men. Lipids. 1999;34:317- 324.
- Savill J, Dransfield I, Gregory C, Haslett A blast from the past: clearance of apoptotic cells regulates immune responses. Nat Rev Immunol. 2002;2:965-975. Review.
- Conti F, Magrini L, Priori R, Valesini G, Bonini Eosinophil cation- ic protein serum levels and allergy in chronic fatigue syndrome. Allergy. 1996;51:124-127.
- Henz BM, Zuberbier Most chronic urticaria is food-dependent, and not idiopathic. Exp Dermatol. 1998;7:139-142. Review.
- H?j Food intolerance in patients with angioedema and chron- ic urticaria: An investigation by RAST and Alcat Test. Euro J of Allergy & Clin Immun. 1995;50 (supplement No. 26).
- Jaffe Delayed allergies in comprehensive care: Enhancing clinical outcomes through functional lymphocyte response as- say in primary management of chronic ill health. The Original Internist. December 2003.
- Marshall JD, Abtahi S, Eiden JJ, Tuck S, Milley R, Haycock F, Reid MJ, Kagey-Sobotka A, Creticos PS, Lichtenstein LM, Van Nest Immunostimulatory sequence DNA linked to the Amb a 1 aller- gen promotes T(H)1 cytokine expression while downregulating T(H)2 cytokine expression in PBMCs from human patients with ragweed allergy. J Allergy Clin Immunol. 2001;108:191-197.
- Keller KM, Bürgin-Wolff A, Lippold R, Lentze [Quality assur- ance in diagnostics: are there normal values for IgG-antibodies to cow’s milk proteins?] Klin Padiatr. 1999;211:384-388. [In Ger- man.]
- Hadjivassiliou M, Grünewald RA, Davies-Jones GA. Gluten sensi- tivity: a many headed BMJ. 1999;318:1710-1711.
- Szabó I, Eigenmann Allergenicity of major cow’s milk and peanut proteins determined by IgE and IgG immunoblotting. Allergy. 2000;55:42-49.
- Jenkins M, Vickers Unreliability of IgE/IgG4 antibody test- ing as a diagnostic tool in food intolerance. Clin Exp Allergy. 1998;28:1526-1529.
- Zar S, Kumar D, Benson Food hypersensitivity and irritable bowel syndrome. Aliment Pharmacol Ther. 2001;15:439-449. Re- view.
- Crocker IP, Wellings RP, Fletcher J, Baker neutrophil func- tion in women with pre-eclampsia. Br J Obstet Gynaecol. 1999;106:822-828.
- Miesel R, Hartung R, Kroeger Priming of NADPH oxidase by tumor necrosis factor alpha in patients with inflammatory and autoimmune rheumatic diseases. Inflammation. 1996;20:427-438
- Karima M, Kantarci A, Ohira T, Hasturk H, Jones VL, Nam BH, Mal- abanan A, Trackman PC, Badwey JA, Van Dyke Enhanced su- peroxide release and elevated protein kinase C activity in neu- trophils from diabetic patients: association with periodontitis. J Leukoc Biol. 2005;78:862-870. Epub 2005 Aug 4.
- Poon BY, Ward CA, Cooper CB, Giles WR, Burns AR, Kubes al- pha(4)-integrin mediates neutrophil-induced free radical injury to cardiac myocytes. J Cell Biol. 2001; 152:857-866.
- Vitte J, Michel BF, Bongrand P, Gastaut Oxidative stress level in circulating neutrophils is linked to neurodegenerative diseas- es. J Clin Immunol. 2004;24:683-692.
- Frey B, Haupt R, Alms S, Holzmann G, König T, Kern H, Kox W, Rüstow B, Schlame Increase in fragmented phosphati- dylcholine in blood plasma by oxidative stress. J Lipid Res. 2000;41:1145- 1153.
- Zhang R, Brennan ML, Fu X, Aviles RJ, Pearce GL, Penn MS, To- pol EJ, Sprecher DL, Hazen Association between myelop- eroxidase levels and risk of coronary artery disease. JAMA. 2001;286:2136-2142.
- Li L, Zhang Y, Chen YG, Li GS, Wang Y, Ma X, Li JF, Zhong M, Zhang [Changes of neutrophil myeloperoxidase in coronary circulation among patients with acute coronary syndrome.] Zhonghua Xin Xue Guan Bing Za Zhi. 2005;33:1106-1108. [In Chinese].
- Duncan BB, Schmidt Chronic activation of the innate im- mune system may underlie the metabolic syndrome. Sao Paulo Med J. 2001;119:122-127.
- Shan L, Molberg , Parrot I, Hausch F, Filiz F, Gray GM, Sollid LM, Khosla C. Structural basis for gluten intolerance in celiac sprue. Science. 2002;297:2275-2279.
- Kotsanis, Paper presented to American Academy of Otolaryn- gic Allergy on a Multi-disciplinary treatment of autistic patients, combining allergy, nutrition, and auditory training. 1993; Data on file at CSS.
- Høj Diagnostic value of Alcat Test in intolerance to food ad- ditives compared with double blind placebo controlled (DBPC) oral challenges. J Alleg Clin Immun. 1996: No 1, part 3.
- Mele Immune Cell Competence following In-Vitro chal- lenge with Alcat Positive Foods [English Translation]. Biotikos, Anno 1o – Numero 1, Giugno 2000.
Current overview of Alcat Test Studies 2014
(Most of these can be downloaded from www.alcat.com)
Double-blind studies:
- High correlation of the Alcat Test Results with Double-Blind Challenge (DBC) in Food Sensitivity by P. Fell, presented at the 45th Annual Congress of the American College of Allergy and Immunology, Los Angeles, CA:November 12-16, 1988 and published in the Annals of Allergy.
- Alcat a new test for food induced problems in medicine? Fell et , presented at the annual meeting of the American Academy of Otolaryngic Allergy, Washington DC, 1st Oct 1988.
- Alcat® – a new cellular test for food sensitivity Fell, Brostoff & Soulsby, presentation of study and results at the annual meet- ing of the American In-Vitro Allergy & Immunology Society, Au- gust 1990, Toronto,
- Cellular responses to food in irritable bowel syndrome – an in- vestigation of the Alcat Test Fell, Soulsby & Brostoff, publication of the summarized study results, Journal of Nutritional Medi- cine, 2, No. 2, 1991.
- Diagnostic Value of Alcat Test in intolerance to food additives compared with double-blind placebo-controlled (DBPC) oral challenges Hoj, J Allerg Clin Immun 1 (3); 1996
Reproducibility Studies:
- Reproducibility of the Alcat Test by Potter, H. Steinmann et al., University of Cape Town, South Africa, 1994
- Reproducibility of the Antigen Leukocyte Cellular Antibody test (Alcat)—Statistical Analysis, Summary Statistics & Scientif- ic Report“, University of the Range Free State in Bloemfontein, Südafrika, WML Neetling and Dr. AM Kachelhoffer von Janu- ar-April, 1998.
- Parexel Medstat Final Statistical Report – Study of the Alcat Test in 10 subjects, Per Fuglerud, Parexel Norwegen, Nov. 1999
- Study Comparing Alcat Test Results With Flow Cytometry and Microscop, Gitte Jensen, NIS Labs (Natural Immune System) Oregon, USA, 2009
Other Alcat Test Studies:
- Evaluation of Alcat Test Results in the Non-IgE Mediated Pathol- ogy of the Skin“ DeAmici et , Study performance and study report at the University of Pavia, Italy. Presented at the 30th Congress of the European Academy of Allergy and Clinical Im- munology, 11-15 June 2011 – Istanbul, Turkey. (Poster Presenta- tion, Abstract #553)
- Alcat Test Results in the Treatment of Gastrointestinal Symp- toms“ Berardi et al., Study performance and study report at the University of Pavia, Italy. Presented at the 30th Congress of the European Academy of Allergy and Clinical Immunology, 11- 15 June 2011 – Istanbul, Turkey. (Poster Presentation, Abstract
- Rational management of food intolerance in an elite soccer club“ Angelini et , Journal of the International Society of Sports Nutrition 2011, 8(Suppl 1):36
- Alcat Test Identifies Food Intolerance in Patients with Gastroin- testinal Symptoms“ Berardi et , Report of the XXVIII Congress of the European Academy of Allergy & Clinical Immunology, European Journal of Allergy and Clinical Immunology, Supple- ment 90, Volume 64, 2009, pg. 490.
- Food Intolerance in Patients with Cutaneous Diseases: Diag- nostic Value of the Alcat Test“ Berardi et , Report of the XXVIII Congress of the European Academy of Allergy and Clinical Im- munology, European Journal of Allergy and Clinical Immunolo- gy, Supplement 90, Volume 64, 2009, pg. 490.
- The Effect of the Alcat Test Diet Therapy for Food Sensitivity in Patients with Obesity“ Akmal et , Middle East Journal of Fam- ily Medicine. April 2009 – Vol. 7, Issue 3.
- IMS Health Economics and Outcomes Research—Influence of Food Intolerance in Migraines: Final Report of Statistical Re- sults“ Immunological Center of Cataluna, Version 3, December 28,
- Ogni intervento comincia a tavola, Mele Cristina, Medici Oggi, Maggio 2002: 210-213
- Controversial antigen leucocyte cellular antibody test (Alcat): a nonspecific inhibitory effect of alpha glycoproteins, Kedryna & Guminska, Med Sci Monit 1999; 5(2):BR193-197.
- A Comparison of the Alcat Test for Food Reactions Amongst 2 Population Sub-Groups“ Study presentation of DH Sandberg et al., 45th Annual Congress of the American College of Allergy and Immunology, Los Angeles, CA: November 12-16, 1998, pub- lished in the Annals of Allergy.
- Outcome Study in 353 Consecutive Patients Following The Alcat Diet“, Study of Lene Hoj in Kopenhagen at the Allergy Clinic Charlottenlund, Denmark 1998. Non-Published.
- Evaluation of the cytotoxic food test and the Alcat, Pol Merkuri- usz 1997 Feb;2(8):154-9.
- South African Outcome Randomized study with 274 pa- tients, Dr. Jan Geldenhuys, Johannesburg, South Africa, 1997
- Technical Study Comparing The Alcat Methodology With Ac- tivation Of Granulocytes Following Challenge With Zymosan, Study of Christina Mele at the University of Rome.
- The Short Term Efficacy of the Alcat Test of Food Sensitivities to Facilitate Changes in Body Composition and Self-Reported Disease Symptoms: A Randomized Controlled Study“ Kaats et in Am J of Bariatric Med, Spring 1996: 18-23.
- El test Alcat de sensibilidad a los alimentos y su interés en Me- dicina Estética Cabo-Soler Alcuni Particolari Della Dieta In Medicina Estetica (Comments On Diets In Esthetic Medicine). Abstract of 14th Med Day of Esthetical Medicine & Dermato- logical Survey. Venice, Italy, Sep. 22-23, 1995. Published in the proceedings.
- Prevalence of food allergy and intolerance in children based on MAST CLA and Alcat Tests“ Buczylko et , Rocz Akad Med Bi- alymst. 1995; 40(3):452-456.
- Alcat Test Results in the Treatment of Respiratory and Gastroin- testinal Symptoms, Arthritis, Skin and Central Nervous System“ Mylek et , Rocz Akad Med Bialymst. 1995; 40(3): 625-629.
- Food Intolerance in Patients with Angioedemia and Chronic An investigation by RAST and Alcat Test. Study of Dr. Lene Hoj, presented at the XVI European Congress of Allergy and Clinical Immunology, Madrid, Spain: June 25-30, 1995, pub- lished in European Journal of Allergy and Clinical Immunology, Supplement No. 26, Vol. 50, 1995.
- “Autism – a multidisciplinary approach to treatment”, Kotsanis et 1994. Study conduction under the direction of Dr. Con- stantine Kotsanis, results presentation at the annual meeting of the American Academy of Otolaryngic Allergy 1994. Study data available for download at www.kotsanisinstitute.com/home/ autism-treatment
- The Alcat Test: in vitro procedure for determining food sensitiv- ities“ Pasula , Folia Med Cracov. 1993;34(1-4):153-7.
- The Alcat Test—A Guide and Barometer in the Therapy of Envi- ronmental and Food Sensitivities BA Solomon, Environmen- tal Medicine, Vol. 9, Number 2, 1992:2-6
- Pilot Study into the Effect of Naturally Occurring Pharmacoact- ive Agents on the Alcat Fell, PJ. American Otolaryngic Al- lergy Association Annual Meeting, September 27, 1991, Kansas City, MO. Published in the proceedings.
- Inhibitory Effect of Sodium Cromoglycate on Granulocyte Re- sponse to Food Antigens In-Vitro. Fell PJ, Sandberg DH et , 47th Annual meeting of the American College of Allergy & Im- munology, November 10-14, 1990, San Francisco, CA. Published in the proceedings.
- Gastrointestinal Complaints Related to Diet, DH Sandberg, In- ternational Pediatrics, 5 No. 1, 1990:23-9.
- Pharmacoactive Compounds in Foods – The effect on the Alcat Test in Healthy volunteers and patients suffering from Migraine Fell PJ, Brostoff J et , AAOA News 9:2:29.
- Multiple Pathogenic Mechanisms in Food Sensitivity Reaction In-Vitro. Puccio SG et , 4th International Symposium on Im- munological and Clinical Problems of Food Allergy, Milan, Italy. November 5-9, 1989. Abstract Symposium Book, pg. 37.
- Influence of Food antigens on Volumes of Circulating White Blood Cells and Platelets Aggregation Studienpräsentation beim Symposium on Immunological and Clinical Problems of Food Allergy, Mailand, Italien, 5.-9. November 1989.
Related Studies
- Sapone, et al: Divergence of gut permeability and muco- sal immune gene expression in two gluten-associated con- ditions: celiac disease and gluten sensitivity. BMC Medicine, 9:23; 2011
- Berardi et al: Alcat Test identifies food intolerance in patients with gastrointestinal symptoms, Clinical Study 2011, Po- liklinik Pavia, Italien
- Fell, et al: Cellular Responses to Food in Irritable Bowel Syn- drome – An Investigation of the ALCAT TEST. Journal of Nutri- tional Medicine, 2, 143-149; 1991
- Berardi et al: Food intolerance in patients with cutaneous diseases: diagnostic value of the Alcat Test. Clinical Study 2011, Department of Dermatology, Pavia, Italien
- Samaroo et al: Novel immune response to gluten in individ- uals with schizophrenia. Schizophr Res, 118:248-55; 2010
- Dickerson et al: Markers of gluten sensitivity in acute mania: A longitudinal study. Psychiatry Res, 196:68-71; 2012
- Rashtak et al: Serology of celiac disease in gluten sensitive ataxia or neuropathy; Role of deamidated gliadin J Neuro-immunol 2011; 230:130-134
- Vitte J et al: Oxidative stress levels in circulating neutrophils is linked to neurodegenerative J Clin Immunol, 24(6):683-92; 2004
- Oodegard JI et al: Connecting Type 1 and Type 2 Diabetes through Innate Cold Spring Harb Perspect Med, 2(3); 2012
- Duncan BB et al: Chronic activation of the innate immune sys- tem may underlie the metabolic Sao Paulo Med J, 119:3; 2001
- Lee Role of innate immunity in diabetes and metabolism: recent progress in the study of inflammasomes. Immune Netw 11:95-9; 2011
- Tremellen K & Tunc Macrophage activity in semen is sig- nificantly correlated with sperm quality in infertile men. Int J Androl 33:823-31, 2010
- Bastard JP et al: Recent advances in the relationship between obesity, inflammation, and insulin Eur Cytokine Netw, 17(1):4-12; 2006
- Miesel R et al: Priming of NADPH oxidase by tumor necrosis factor alpha in patients with inflammatory and autoimmune rheumatic diseases. Inflammation, 20(4):427-38; 1996
- Fitzpatrick AL et al: Leukocyte telomere length and cardiovas- cular disease in the cardiovascular health Am J Epide- miol 165:14-21; 2007
- Tlaskalova-Hogenova et al: Involvement of innate immunity in the development of inflammatory and autoimmune diseas- Ann N Y Acad Sci,1051:787-98; 2005
- Zhonghua et al: Changes of neutrophil myeloperoxidase in coronary circulation among patients with acute coronary syn- 33:1106-8; 2005
- Wan-Wan L Al: A cytokine-mediated link between innate immunity, inflammation and cancer. J Clin Invest, 117(5):1175- 1183; 2007
- Poon BY et al: alpha(4)-integrin mediates neutrophil-induced free radical injury to cardiac J Cell Biol 152(5):857- 66; 2001
- Samaroo D, al. Novel immune response to gluten in indi- viduals with schizophrenia. Schizophr Res. 2010 May; 118(1- 3):248-55.